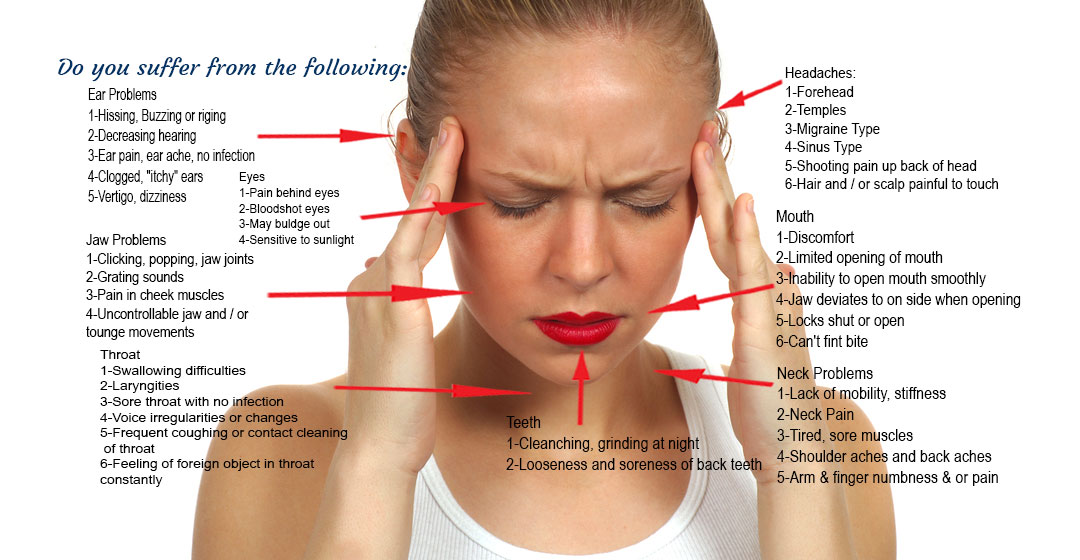
The jaw plays a crucial role in the overall structure and functioning of the head and neck. When issues arise with the jaw, it can lead to headaches and neck pain. Here are some ways jaw problems can cause these symptoms:
Covid Clenching & Bruxism: “Covid Clenching” or Bruxism Teeth Grinding, Facial Pain Have Increased Due to Stress from COVID-19. Scientists have found that many people experience increased teeth grinding and pain during the COVID-19 pandemic. This is most likely due to the pandemic stress and anxiety. If you have dealt with more dental symptoms, such as teeth grinding, jaw clenching, and jaw pain during the COVID-19 pandemic, this probably isn’t just a coincidence. Times of stress and anxiety can lead to adverse health effects like temporomandibular disorders (TMD) and bruxism (teeth grinding). Anyone who’s under stress is likely to experience jaw clenching and teeth grinding. As reported on national media - People are under immense stress during the Covid-19 pandemic, and it’s showing up on people’s teeth. The American Dental Association found that 63 percent of dentists have seen teeth cracked as a result of grinding or clenching their teeth at night.
Temporomandibular Joint (TMJ) Disorder: The TMJ connects the jawbone to the skull. TMJ disorder occurs when this joint malfunctions or misaligns. It can be caused by various factors such as teeth grinding, jaw clenching, arthritis, or injury. When the TMJ is affected, it can cause pain in the jaw, face, and temples, and even radiate to the head, leading to headaches.
Muscle Tension and Spasm: Chronic muscle tension in the jaw, typically associated with bruxism or teeth grinding, can strain the surrounding muscles. This excessive muscle activity can cause headaches, often called tension headaches. The muscles involved in jaw movement are closely interconnected with the muscles of the head and neck, so tension and spasms in the jaw muscles can refer pain to the head.
Trigeminal Nerve Irritation: The trigeminal nerve is a major nerve responsible for carrying sensory information from the face to the brain. When the jaw is misaligned or experiencing excessive pressure, it can irritate the trigeminal nerve. The sensory nerves of the head & face travel near to or through the different muscle groups that control the jaw. When the jaw joint is not in harmony, the tension created in the muscles can put pressure on these nerves & cause them to become irritated over time. This irritation can result in referred pain, including headaches and facial pain.
Dental Issues: Problems with the teeth, such as malocclusion (misalignment), tooth decay, or abscesses, can cause referred pain to the head. Dental issues can affect the jaw alignment and functioning, leading to headaches and facial discomfort. It's worth noting that stress and anxiety can exacerbate jaw-related issues, as they often contribute to teeth grinding and jaw clenching. The resulting muscle tension and strain can lead to headaches.
If you're experiencing persistent jaw pain or headaches, it's advisable to consult with a healthcare professional, such as a dentist or a doctor specializing in orofacial pain. This professional can evaluate your specific symptoms, perform an examination, and provide appropriate diagnosis and treatment options.


First, Dr. Hlavaty examine the joint, the jaw and how they operate to determine if there is any damage to the joint and to identify if there is dysfunction in the joint itself. He will then examine the muscles that control the jaw & check out how the teeth fit together.

To properly evaluate the TMJ, Dr. Hlavaty will take X-rays & sometimes a CT scan will be needed to see inside the joint to help determine if there is interior damage to the bony structures of the jaw.

Once Dr. Hlavaty has determined the source of the problem or problems affecting the jaw & causing the pain or discomfort, he will put together a treatment plan with various options to address the underlying problems & help to get you out of pain

Dr. Hlavaty will send you home with instructions on how to properly take care of the issues. Depending on the types of treatments prescribed, there may be need for multiple treatments over a period of time. These treatments may include oral appliances, bite adjustment or rebuilding, muscle relaxation exercises, electrical muscle stimulation, injections of medications, or referral to a surgeon if there is severe structural damage to the joint.
An oral deprogramming appliance, also known as a bite splint or orthotic, is a dental device used to relax and reposition the jaw muscles and joints. It is primarily used in the treatment of temporomandibular joint (TMJ) disorders and related conditions.
The appliance is typically made of acrylic material and custom-fitted to the patient's mouth by a dentist or a dental specialist. It is designed to temporarily alter the bite and provide a more stable and relaxed jaw position. The specific design of the appliance may vary depending on the individual's needs and the intended treatment goals.
The primary function of an oral deprogramming appliance is to reduce muscle tension, relieve pressure on the jaw joints, and promote a more balanced bite. By repositioning the jaw and allowing the muscles to rest in a more relaxed state, it can help alleviate symptoms such as jaw pain, headaches, facial discomfort, and teeth grinding.
The use of an oral deprogramming appliance is often part of a comprehensive treatment approach for TMJ disorders. It may be used in conjunction with other therapies, such as physical therapy, stress management techniques, and lifestyle modifications.
The NTI TSS+ (Nociceptive Trigeminal Inhibition Tension Suppression System Plus) appliance is a specialized type of oral splint used in the treatment of temporomandibular joint (TMJ) disorders, migraines, and tension headaches. It is a small, custom-fitted device that is typically worn over the front teeth during sleep.
The NTI TSS+ appliance differs from traditional oral splints in its design and function. It consists of a small, clear, horseshoe-shaped device that covers only the front teeth (either the upper or lower). The appliance is designed to create a separation between the back teeth, preventing full contact and reducing the intensity of jaw clenching and grinding during sleep.The primary purpose of the NTI TSS+ appliance is to inhibit the intensity of muscle contractions and reduce the overall force on the temporomandibular joint. By preventing the back teeth from coming into full contact, it helps to relax the muscles of the jaw, relieve tension, and minimize the harmful effects of clenching and grinding, which can contribute to TMJ disorders and headaches.
Adjustment of the occlusion, also known as occlusal adjustment or bite adjustment, can help relieve TMJ (temporomandibular joint) symptoms by achieving a more balanced and harmonious bite.
Here's how it works:
Alignment of the Teeth: Occlusal adjustment involves selectively reshaping or adjusting specific areas of the teeth to ensure proper alignment and contact during biting and chewing. By improving the way the upper and lower teeth fit together (occlusion), it can reduce excessive forces and stress on the TMJ.
Distribution of Forces: Uneven or imbalanced contact between the teeth can cause certain areas of the jaw to bear more force than others, leading to muscle tension and joint strain. By redistributing the forces evenly across the dental arches, occlusal adjustment can help alleviate excessive pressure on the TMJ and surrounding structures.
Muscle Relaxation: A misaligned bite can result in overactive or strained jaw muscles as they try to compensate for the imbalances. By achieving a more stable and harmonious bite, occlusal adjustment can help relax the jaw muscles, relieving muscle tension and reducing associated TMJ symptoms.
Joint Positioning: Occlusal adjustment can also influence the positioning of the TMJ itself. By optimizing the way the jaw joint sits within its socket, it can promote better joint stability, reduce friction and wear, and alleviate discomfort.
It's important to note that occlusal adjustment is a precise and delicate procedure. The process typically involves a comprehensive evaluation of the bite, careful analysis of the dentition, and the use of instruments to make precise adjustments. Dr. Hlavaty will assess your specific symptoms, evaluate your bite relationship, and determine if occlusal adjustment is a suitable treatment option for your TMJ condition. In some cases, occlusal adjustment may be combined with other treatments such as oral splints, physical therapy, stress management techniques, or orthodontic interventions to achieve optimal results.
Botox (Botulinum toxin) can be used as a treatment option for managing TMJ (temporomandibular joint) issues, bruxism (teeth grinding), and headaches.
Here's how Botox is used in each case:
TMJ Issues: Botox injections can help alleviate TMJ-related pain and muscle tension. When injected into the jaw muscles, Botox blocks the release of acetylcholine, a neurotransmitter responsible for muscle contraction. By temporarily relaxing the muscles, Botox can reduce muscle hyperactivity, relieve jaw pain, and improve jaw function in individuals with TMJ disorders.
Bruxism: Botox injections can be used as a therapeutic option for managing bruxism, a condition characterized by clenching or grinding of teeth. By injecting Botox into the muscles involved in jaw movement, such as the masseter and temporalis muscles, it can help reduce the intensity and frequency of involuntary muscle contractions associated with bruxism. This can lead to a decrease in teeth grinding and its related symptoms.
Headaches: Botox injections can also be used to manage headaches, particularly chronic migraines. The exact mechanism of how Botox helps with headaches is not fully understood, but it is believed to involve the inhibition of pain signals transmitted by sensory nerves. Botox injections are typically administered in specific areas of the head and neck, such as the forehead, temples, and neck muscles, targeting trigger points associated with migraines and tension headaches.
Botox treatment is temporary and usually requires repeated sessions to maintain its effectiveness. The duration of relief can vary among individuals, but the effects of Botox typically last for several months. Regular follow-up appointments will be necessary to monitor the response to treatment and determine the need for subsequent injections. As with any medical procedure, Botox treatment carries potential risks and side effects, which should be discussed with Dr. Hlavaty before proceeding. He will provide you with detailed information about the benefits, potential risks, and expected outcomes based on your individual circumstances.
Dental sealants are most commonly recommended for children who may be high-risk for tooth decay, but they’re also a great option for patients of any age who wish to protect themselves from developing cavities. A relatively straight-forward procedure, dental sealants start with the application of dental resin, usually to the rear teeth, as they have more grooves and uneven surfaces where plaque and bacteria can easily hide. A UV light will be used to cure the resin, hardening it and creating a powerful barrier between your enamel and food debris, acid, or bacteria. When applied correctly, dental sealants can last for years!
Many patients struggle with gum disease, and if left untreated, can risk losing their teeth and other problems. Gingivitis is the first stage of gum disease, and is the only stage that can actually be reversed with deep cleanings and attentive at-home hygiene. If you have gum disease, keeping up with your regular cleanings and checkups will help you gain control over your oral health before it’s too late!
For patients with more advanced stages of periodontitis, we recommend scheduling deep cleanings at more frequent intervals, usually every three to four months. Although the effects of advanced gum disease can’t be reversed, deep cleanings, scaling, and root planing can halt the progression of periodontitis and help preserve your oral health.
Oral cancer screenings are an important part of every preventive care visit. Catching oral cancer in its early stages allows us to stop it before it spreads, and can save your life. That’s why we’ll always check for signs of oral cancer at every preventive visit.
Your dentist will examine your oral tissues, like your gums and tongue, keeping an eye out for abnormalities like lesions, lumps, discolorations. If we find anything unusual, we’ll take a biopsy and send it out to a specialist for a thorough analysis. Although oral cancer isn’t overly common, it’s important to remain proactive and consistent with your oral healthcare routine, so we can identify any issues before they become major problems.
Teeth grinding and clenching while sleeping is a common issue faced by many patients. Night guards are a great solution for this unconscious clenching, also known as bruxism. Night guards form a soft barrier that protects your teeth from damage caused by the pressure of clenching and grinding. Your dentist will take an impression or a scan of your teeth and gums to create a unique mold that will be sent to a dental lab, where your night guard will be custom-crafted. Night guards work by easing the tension in your jaw, alleviating the painful headaches and other side effects of clenching and grinding, so you can get the sleep you need and keep your teeth from wearing down.
Sports mouth guards are worn over the teeth, just like night guards. However sports guards are designed specifically to protect your smile from dental injuries that are so common when playing high-intensity impact sports. Custom-fitted sports guards can help protect athletes from oral trauma caused by collisions to the mouth, face, and head. If you play football, basketball, baseball, soccer, rugby, hockey, gymnastics, mountain biking, or other activities that put you at risk for injury due from falls, body contact, or flying objects, ask us about getting fitted for a custom sports guard today! Tailored to fit your unique smile, sports guards are comfortable, durable, and won’t stop you from playing the sports you love.
Patients often ask about the long-term outlook for TMJ treatment. While there may or may not be a definitive cure for your specific issues, we can provide information on managing symptoms and improving jaw function over time. In a lot of cases we can correct the underlying problems, but that usually requires the functional rebuilding of the occlusion (bite). This typically requires a combination of crowns/veneers/fillings that are built to guide the jaw into its proper anatomical positioning thus taking the stress off the joint & surrounding musculature. This is a great option for some patients, but can be difficult for some due to financial constraints. In cases where correcting the underlying issues is not feasible, we focus on management of the symptoms, allowing patients to return to a normal pain-free life.